Steven Tuttle has cycled through addiction, homelessness, recovery and housing so many times that it’s hard to reconstruct the journey that led him to Fort Lyon.
It started in West Denver in the late 1970s, where Tuttle snorted (and dealt) a lot of cocaine as a teenager. A gunfight and an arrest scared him straight, and by his mid-20s he had a wife, two kids and a decent job painting houses.
When his wife died in a car crash, Tuttle relapsed hard. He started freebasing cocaine, lost his job and wound up living on the streets. A stint in residential recovery got him back on his feet, and he stayed clean until his brother got shot and nearly bled to death in Tuttle’s arms. That brought on another relapse and sent Tuttle drifting between the streets, Denver detox, and a hodgepodge of treatment programs that included 12-step centers, peer mentoring, trauma counseling and cognitive therapy.
These interventions were too fleeting, and Tuttle’s life too unstable, to yield lasting progress. Likewise, his transient existence made it almost impossible to address the physical ailments that piled up over time. Tuttle limped along with bulging disks, sciatica, torn rotator cuffs, a balky ankle and more, with occasional band-aid treatment in ERs and clinics. When he developed persistent flu-like symptoms, they weren’t recognized as spinal meningitis until it was almost too late—Tuttle spent six weeks in a coma. Later, he contracted endocarditis (an infection of the heart lining), which went undiagnosed until Tuttle suffered two heart attacks.
“The doctors told me I needed to stop doing drugs,” Tuttle says, “and I knew I needed to stop. I wanted to. But I’ve been doing the same thing for 40 years.”
The Fort Lyon Supportive Residential Community may represent his last, best chance to break the cycle. Located at a former Veterans Administration hospital 80 miles east of Pueblo, on Colorado’s remote southeastern prairies, Fort Lyon is designed for people like Tuttle—chronically homeless individuals with deep-rooted addictions, mental health challenges and physical infirmities. Funded by the state Department of Local Affairs (DOLA) and operated by the Colorado Coalition for the Homeless (CCH), Fort Lyon represents one of Colorado’s most ambitious attempts to tackle the problem of homelessness—and one of its most closely watched. If it can redeem people like Steven Tuttle, Fort Lyon could point the way not only toward better housing policies, but also toward greater health equity.
“Fort Lyon is meant for people who need more than just rental assistance to get off the streets,” says Zac Schaffner of DOLA’s Office of Homeless Initiatives. “We can’t just take individuals who have high barriers to housing stability and stick them in apartments without ensuring they have access to case management, community resources, mental health and other supportive services.”
James Ginsburg, Fort Lyon’s executive director, states the facility’s premise more bluntly: “Housing is health care. This program isn’t just about getting people into housing. It’s about giving sick people a chance to get well.”

Frank Harvey, left, Ron Eslinger, center, and Derrick Ogman chat under a tree near their residence hall at Fort Lyon.
The relationships among homelessness, addiction and health haven’t been easy to document with precision, mainly because it’s so difficult to gather reliable data about a population that’s transient by definition. But the best estimates are as grim as you’d expect.
A 2015 study concluded that 89 percent of people experiencing homelessness have at least one chronic medical condition, 71 percent suffer from mental illness or post-traumatic stress, 59 percent are contending with a long-term addiction, and 39 percent (including Steven Tuttle) are dealing with all three of these conditions simultaneously—a confluence ominously referred to as “tri-morbidity.”
Another investigation (after controlling for income, age and other variables) found that people experiencing homelessness are five times as likely to be alcoholic as people who have housing, three times as likely to have liver disease, twice as likely to have a mental illness, twice as likely to suffer from malnourishment, and 50 percent more likely to have multiple chronic health conditions.
And an international study covering eight major cities in the United States, Canada and Europe calculated that a homeless individual is 40 percent more likely to die on any given day than a housed individual of comparable age and socioeconomic status.
Those trends are mirrored in the best Denver data source, the Metro Denver Point-in-Time Survey compiled by the Metro Denver Homeless Initiative. That annual study’s most recent edition estimated that among the 5,315 people who experience homelessness locally on any given night, 27 percent suffer from mental health issues and 29 percent have substance abuse problems. A subset of that population—about a third of the total—is defined as “chronically homeless,” meaning that—like Steven Tuttle—they’ve experienced homelessness continuously for at least a year, or recurrently over a period of years.
That subset of the population has increased 60 percent in Colorado since 2010, and its health markers are more dire. Within metro Denver, nearly 60 percent of chronically homeless individuals are disabled, 57 percent suffer from mental illness, 46 percent are habitual substance abusers, and 38 percent have other chronic health problems. Statewide, Colorado has around 2,264 chronically homeless individuals, which ranks seventh most among the 50 states.
Statistics like these moved two Harvard experts to argue that “addressing the medical issues of homeless people is the health equity challenge of our time.”
Writing in the Journal of the American Medical Association, physicians Howard Koh and James O’Connell noted that persons experiencing homelessness routinely face “a complex burden of simultaneous medical, mental health, and substance abuse problems” that reinforce—and are, in turn, reinforced by—housing instability. Irregular diets and chaotic routines cause otherwise manageable conditions such as diabetes and hypertension to fester unchecked. Bacterial and viral ailments such as bronchitis flourish in bad weather, and spread quickly in overnight shelters. Poor hygiene decimates teeth and breeds lice, fungi and skin rashes. The sheer physical burdens of homelessness—hauling possessions around, walking everywhere, constantly living (often sleeping) on concrete—are brutal on backs, necks, feet and joints.
“Obviously, being exposed to harsh weather and all the elements can have severe health consequences,” says Mary Cunningham, a senior fellow at the Urban Institute who focuses on housing and homelessness. “But lack of access to health care is the bigger impact. These are people who are in and out of the emergency room. They can’t really get preventative care or treatment for long-term or chronic illnesses.”
“They sit in long lines,” adds Christina Carlson of Urban Peak, a Denver-based nonprofit that serves homeless youth. (Urban Peak is a past grantee of The Colorado Trust.) “They run out of meds, or their meds are expired. Maybe they can’t get the benefits they’re eligible for because they don’t have a driver’s license or a birth certificate. Or they don’t even apply for benefits, because they’ve been failed by the system so routinely.”
All these factors help explain why piecemeal solutions haven’t been effective in getting people like Steven Tuttle off the streets permanently. “The population we’re serving tends to have co-occurring problems,” says Lisa Thompson, CCH’s chief operating officer. “You can’t just focus on one thing. You need to address everything at once—and that can make the problem seem so overwhelming that people believe it can’t be solved.”
Enter Fort Lyon. Established in 2013, it integrates multiple forms of support in a holistic package. Fort Lyon residents live rent-free in dormitory-style housing, with all meals included. They have on-site access to addiction counseling, peer mentoring, basic preventative health care and prescription medications. Treatment for more serious health problems and mental disorders (including PTSD) is available at partner facilities in Pueblo, Lamar and Las Animas. Being housed and sober enables Fort Lyon residents to receive sustained, coordinated medical treatment instead of the intermittent, incomplete ER fixes they typically got while homeless.
Beyond basic necessities like food, shelter and health care, Fort Lyon provides activities and amenities that are designed to steer participants into constructive behaviors that support self-sufficiency. Residents can take community college classes, develop work skills, get job experience and even launch independent ventures. One former resident established a bicycle shop on campus, restoring old junkers that participants can ride to and from nearby Las Animas. Another resident operates a barber shop on campus. Others maintain the onsite woodworking shop, operate the library, and organize softball games, pool tournaments and movie nights. Fort Lyon recently opened a storefront on Main Street in Las Animas where residents sell art, clothing and other products.

Tommy Suska sews a band onto a cowboy hat in the sewing room.
None of this programming is unique to Fort Lyon; Tuttle had access to similar types of support over the years. But he could never get it all at one time, in one place—nor, crucially, at a facility as well-resourced as Fort Lyon. Funded annually by $5 million in state dollars, Fort Lyon can support residents’ recovery with more generous helpings of time, space and independence than most nonprofit programs could afford. Participants can stay for as long as three years, a far lengthier interval than the three- to six-month limits most residential recovery programs impose. They also can roam a sprawling, pastoral campus, one that’s far removed (both in distance and in form) from asphalt jungles.
“It’s out in the middle of nowhere,” says Jason Sweeny, “away from everything I’m used to. That seclusion is really important for recovery, especially in the beginning.”
A self-described “trash-can addict” who abused heroin, methamphetamine, alcohol, LSD and whatever else he could get his hands on, Sweeny is about 20 years younger than Tuttle and has a shorter backlog of deferred health care. But he’s still had plenty of struggles trying to take care of his health.
“You’re sleeping in the elements,” he says of being homeless, “so a little chest congestion can last three months. I had really bad chest congestion, and they just gave me a nebulizer in the ER and referred me to a specialist in way-out Aurora, which is really hard to get to when you’re homeless. Maybe it’s just that ER personnel are jaded, but if you’re homeless and sick, they give you some vitamins and antibiotics and then they kick you out. If you’re seeking pain relief, even if you have a legitimate need—like, let’s say you have a broken jaw [which Sweeny once did]—they won’t give you anything stronger than Tylenol. They think it’s drug-seeking behavior.”
Sweeny got to Fort Lyon after numerous failed attempts at rehabilitation in other programs. Fort Lyon is different, he says, in the degree to which the program encourages residents to guide their own healing.
“When I got here,” he says, “the first thing I was told was: Take 30 days to let your body recuperate. Get the poison out of your body. Get your three squares [meals] a day, get eight hours of good sleep every night, and let your body physically recover. Most places won’t let you do that. They’re very regimented, very structured, and that was never good for me. It produced anxiety and triggered my need to get high.”
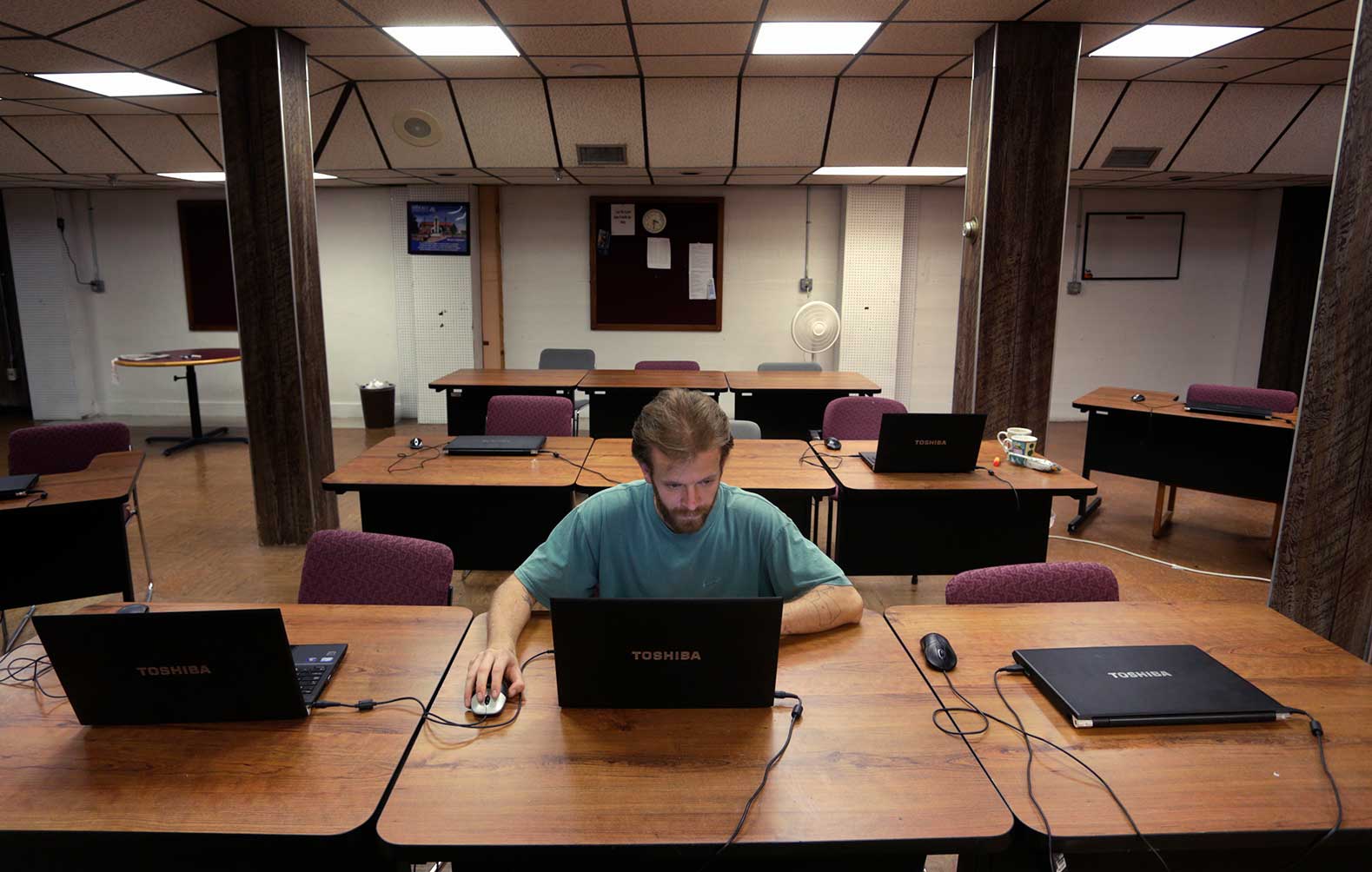
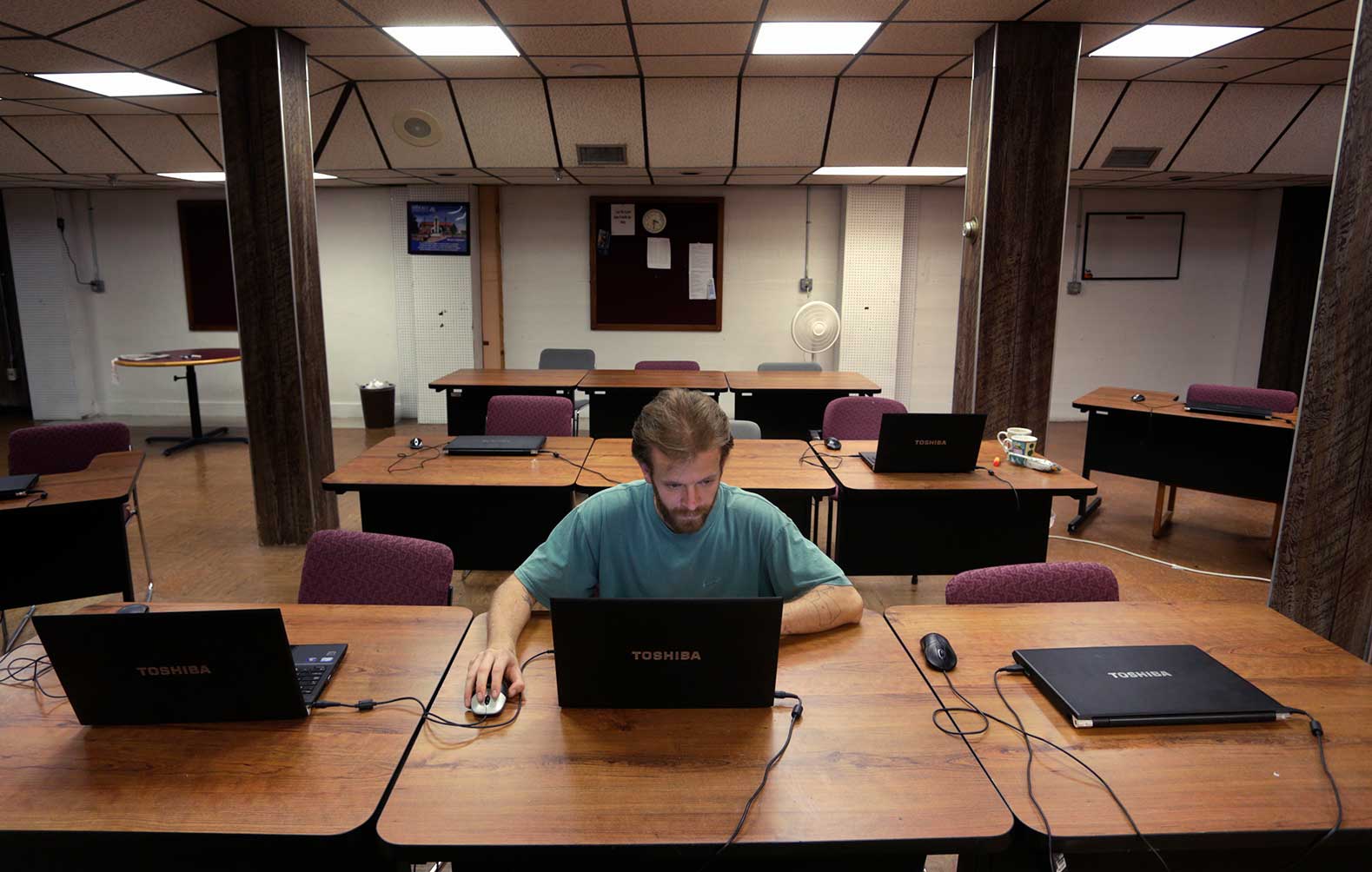
After spending several months at Fort Lyon—sober and drug-free—Sweeny enrolled at Otero Community College so, he says, “I can get into a career that enables me to have my own housing. I feel like I’m in control of my own future. I’m going to be in a better place when I leave here than when I walked in.”
Likewise, Tuttle reports feeling healthier at Fort Lyon than he has in a long time. Although he’s walking with a cane and breathing from an oxygen tank, he says: “I have something over my head. I’m not sleeping in the cold. I’m not getting high, not having to be paranoid. Some days I’m up on my health, and some days I’m not. But I’m doing it on my own terms. I can fix myself here. I just need some structure and an opportunity.”
Ginsburg is justifiably gratified by such comments. “It can seem miraculous,” he says. “You see people rising from the dead emotionally and physically.” But he’s been working with people recovering from addictions for too long to mistake interim progress for permanent success.
During more than a decade as head of the Denver Housing First Collaborative (DHFC), Ginsburg helped thousands of people make the transition from homelessness into permanent housing. About 80 percent of the DHFC’s clients stayed housed and healthy over a period of years. But roughly 20 percent ended up back on the streets—or, worse, died in DHFC housing from an overdose or other factors related to substance abuse.
That 20 percent slice makes up the bulk of Fort Lyon’s population.
“Addiction is a chronic, progressive disease,” Ginsburg says. “They can be at Fort Lyon for three years, which seems like a long time. But we’re seeing people who’ve been using and drinking for 30 years. If they can stay clean here for three years, that’s just the start. Long-term recovery is defined as five years. Only 15 percent of chronic substance abusers ever achieve it.”
It’s impossible to say whether Fort Lyon is meeting or exceeding that standard. To begin with, the program just observed its fifth anniversary, so the five-year threshold hasn’t even arrived yet for most of the 900 people who’ve been housed at Fort Lyon since its inception. But on a more fundamental level, DOLA and CCH lack the means to track long-term outcomes systematically. A person might leave Fort Lyon sober and move straight into a job and an apartment, but there’s no mechanism for determining whether—and for how long—that individual stays clean.
“How are you sure they’re landing back on their feet?” asks state representative Jonathan Singer, who co-sponsored the legislation authorizing the Fort Lyon program. “The data are incomplete because it’s such a challenging population. If they return to being homeless, they’re not easy to find.”
Singer, a social worker who chairs the Colorado General Assembly’s Public Health Care & Human Services Committee, describes himself as both a supporter and a skeptic of Fort Lyon. “It’s a brilliant idea for how to help a population that hasn’t been successful in other places,” he says. “CCH has created a supportive environment where people know they won’t be rejected, and they have access to resources they wouldn’t get elsewhere. There’s some really exciting upside.
“But they’re separated from the community that triggered their addictions. Once they return to that community, will they fall back into their addiction? How well-prepared are they to succeed in the long run? We don’t have the data to answer that question.”
However, there is some data available via an independent audit the state legislature mandated to evaluate Fort Lyon’s cost-effectiveness. According to a preliminary draft released last fall, roughly 40 percent of those who’ve left the facility to date achieved “program completion,” an ambiguous term. “Participants self-determine when they have completed the Fort Lyon Program,” the audit notes, “using their progress in meeting their Goals and Outcomes Plan as a guide.” The upshot is that 60 percent of the people who come to Fort Lyon depart with some (or all) of the same challenges they arrived with.
Unfortunately, that cohort includes Steven Tuttle. He left the program earlier this summer for undisclosed reasons. Patient privacy laws constrain Fort Lyon from offering any details, but a source who knows Tuttle said that he has returned to Denver—and fallen back into his addiction.
Among those who do complete the program successfully, 83 percent have exited to stable housing. That’s nothing to sniff at. It means that somewhere around 250 very sick people recovered their health and got a new lease on life at Fort Lyon. But does that outcome justify the roughly $5 million taxpayers spend each year on the program?
“It’s a legitimate question,” Ginsburg says. “I ask myself the same thing: Is this the most judicious use of five million dollars? Could we accomplish more, help more people, if we just spent the same amount of money on rental vouchers and affordable housing?”
Of course, there’s no guarantee the legislature would ever spend $5 million a year on rental vouchers and affordable housing. Singer was able to win support for Fort Lyon in part by showing the program would save money in the short-term. One chronically homeless person who’s living on the streets costs the taxpayers about $46,000 a year in emergency room visits, overnight shelter, incarceration, law enforcement and other social services. It costs less than half as much—about $20,000—to house the same person at Fort Lyon for a year.
But Singer fears that support will dry up if the program can’t prove that it’s achieving its core mission.
“When we have our next economic downturn, will DOLA be able to make a strong enough argument that Fort Lyon is a good use of money?” he asks. “Or are we going to have to cut the program because there’s insufficient data? There are people in the Capitol who never wanted to see Fort Lyon happen because of the cost, or because they believed it wasn’t the best way to help this population. We’ve had the luxury of strong budgets since 2013, so tough choices haven’t been forced.
“It may not survive if we aren’t sure we’re getting the best value for the money,” Singer adds. “I want to see it succeed.”