
The interior of Centennial Correctional Facility South in Cañon City. Photographed in July 2019. Photo by John Herrick
The interior of Centennial Correctional Facility South in Cañon City. Photographed in July 2019. Photo by John Herrick
Last summer, Matthew Harter, a 50-year-old from Lakewood, Colo., was incarcerated at Centennial Correctional Facility South, a prison in Cañon City, when he started to have trouble breathing.
Harter didn’t have COVID-19. He had anxiety, he said, because he was in quarantine, alone in his cell, which was about the size of a parking space, for 23 hours per day, sometimes all day.
Weeks turned to months. His television and crossword puzzles didn’t help. He did jumping jacks to try to tire himself out so he could sleep. His mind was still spinning. He asked to see a physician to discuss his mental health. A physician never showed up. One day, Harter laced up his boots and started kicking the door.
In the end, Harter said he was in quarantine for 82 days. Ten days before he got out, he said, a nurse gave him mirtazapine, a medication for anxiety and depression.
“I don’t sit around inside. I’m an outside person,” Harter said over the phone after he was transferred to a prison in Denver. “I’m gonna have to see a therapist about this when I get out.”
In an effort to slow the spread of COVID-19, the Colorado Department of Corrections isolated inmates in single-person cells nearly all day, sometimes for weeks or months on end, according to a December 2020 report by the department. Such pandemic precautions may have saved lives, but the forced quarantines of inmates to avoid COVID-19 exposure, as well as the medical isolations of inmates believed to have COVID-19, undermined years of work aimed at making prisons feel less traumatic. This work included limiting the use of solitary confinement, a form of punishment regulated in Colorado because of the psychological harm it can cause.
In some cases, people spent longer in isolation or quarantine than what is widely considered the maximum amount of time allowed under the Department of Corrections’ solitary confinement policy, which requires prison officials to offer people at least one hour out of their cell every day and generally requires special approval to keep someone confined to their cell for more than 15 days.
According to the report, the Department of Corrections said that from March 11 to Dec. 18, 2020, some inmates in Centennial South spent 90 days in quarantine and were offered four hours out of their cells every three days. The department used Centennial South as an intake facility during the pandemic because its single-person cells made it easier to quarantine people. Annie Skinner, a spokeswoman for the department, said some inmates may have spent longer in Centennial South because the department didn’t want to transfer someone to another prison with a COVID-19 outbreak.

The exterior of Centennial South in July 2019. Photo by John Herrick
Such prolonged stays in quarantine were common in other prisons. In the Fremont Correctional Facility, also in Cañon City, the average quarantine lasted 52 days due to “recurring positive tests,” according to the report. Fremont had 760 confirmed COVID-19 cases by the end of 2020. Incarcerated people were offered at least 40 minutes out of their cells every other day. In the prison in Buena Vista, the average quarantine lasted 50 days. People were offered about an hour out of their cells each day.
In a federal lawsuit filed against state officials in January 2021, Henry Lee Griffin, Jr., who was sentenced to life in prison for a series of abductions and rapes in the 1990s, alleged the state violated his Eighth Amendment protections against cruel and unusual punishment when, he said, he was locked in a cell at the prison in Buena Vista for more than 23 hours per day for more than 60 days. A federal judge dismissed the lawsuit in early April because Griffin did not pay $402 in filing and administrative fees.
In most prisons, incarcerated people who tested positive for COVID-19 spent 14 days in medical isolation. But at the Limon Correctional Facility, people spent an average of 21 days in medical isolation and were allowed out of their cells for at least one hour each day, according to the Department of Corrections report. Limon reported 544 confirmed COVID-19 cases by the end of last year.
Colorado state lawmakers this year passed a bill that restricts the ability of sheriffs and local jails to put people into solitary confinement (also referred to as “restrictive housing”) and requires them to track how many people in jails are incarcerated in solitary confinement and for how long. The legislation would not apply to state prisons.
Aside from the December 2020 report, which lawmakers requested from the Department of Corrections, the department does not track or maintain a record of how long people are kept in quarantine or medical isolation, according to Adrienne Sanchez, associate director of legal services at the department. The department also doesn’t track aggregate data on how many people are in solitary confinement, or for how long.
In the absence of data, Dean Williams, the executive director for the Department of Corrections, said he could not respond to individual allegations of long-term quarantine or isolation because he did not know the accuracy of such claims.
“If somebody was kept longer than necessary, then I need to review it in the context of the pandemic,” Williams said in a recent interview. “There could be one-off situations.”
Williams said it was a difficult decision to restrict the movement of incarcerated people. One of his top priorities is to make prisons feel less punitive. The COVID-19 restrictions were designed to protect inmates, not punish them, he said.
“We still lost 29 men. That weighs on me,” he said. “The reality is I know we saved lives.”

Dean Williams, the executive director of the Colorado Department of Corrections. Photographed in July 2019. Photo by John Herrick
“I feel like I’m being punished”
The mandated quarantines were among the few tools Williams had to control the spread of the coronavirus in a historically crowded prison system where social distancing is nearly impossible.
Colorado Gov. Jared Polis generally opposed demands from public health experts and advocates to release more people from prison during the pandemic. Instead, through executive order, Polis allowed prison officials to stop accepting people waiting in county jails ahead of their prison sentences and asked police to issue more summons in lieu of arrests. This contributed to the inmate population dropping from 19,357 in March 2020 to 15,490 in April 2021, a decline of about 20%.
Even with the extra space, the disease still infected nearly 9,000 people incarcerated in Colorado prisons, according to the department. Colorado’s infection rate among inmates is 5.5 times the state population’s rate, according to an analysis by the Marshall Project, a nonprofit journalism organization. Since March 2020, 29 people in the Department of Corrections’ custody have died with COVID-19.
Contributing to the severity of the outbreaks was the controversial decision by Polis not to prioritize Colorado’s incarcerated population for the COVID-19 vaccine. The decision defied recommendations from public health experts.
And the quarantines and isolations did not stop the outbreaks, in part because correctional officers likely brought the coronavirus back into prisons on more than one occasion. At times, guards didn’t wear required and readily available masks and other personal protective equipment, sometimes in quarantine and medical isolation units, according to internal audits of correctional facilities such as Buena Vista, Arkansas Valley and Trinidad that were obtained through Colorado’s open records laws. Some prison staff also failed to screen visitors, according to the audits. The Department of Corrections screened staff for COVID-19 using temperature checks for at least three months into the pandemic, before transitioning to more consistent COVID-19 prevalence testing across multiple facilities in July 2020.
Infections, including among prison staff, also prevented people from being transferred to halfway houses, which are privately operated facilities used to transition people out of prisons. Halfway house operators and state officials can agree to incarcerate people in this lower level of supervision at their discretion. But in November 2020, Skinner, of the Department of Corrections, said the department restricted transfers in order to protect the “health and safety of the inmates and the community.” That month, nearly 400 inmates had been approved for a transfer to a halfway house but were still in prison, according to data compiled by the Department of Corrections.
Last year, Timothy Martinez, a 25-year-old from Montrose, was incarcerated in Sterling, the state’s largest prison and the facility with the largest COVID-19 outbreak to date. Martinez said he was eligible to be transferred to a halfway house in December 2019, but said his release was delayed almost a year in part due to outbreaks in Sterling.
“I feel like I’m being punished. It’s a mental roller coaster. It plays with your mind. I’m used to being out all day. I’m used to being working in the community,” Martinez, who worked as a firefighter on the State Wildland Inmate Fire Team crew, said in September last year. “I was at a really high point in my life when I was firefighting. I was proud of myself.”
The following month, his release was delayed again for two weeks after a guard tested positive for COVID-19.
“I just feel trapped,” he said. “Just two weeks. Just two weeks. Just two weeks. I’m about to get to a year.”
The mental toll of the quarantines and isolations prompted some people to hurt themselves, according to one incarcerated person.
“It’s like being in a prison inside a maximum prison. There’s more girls cutting or they’re getting on medication, like myself, just to deal with everything,” wrote Chataignier McCaffrey-Pickett, a 27-year-old incarcerated in the Denver Women’s Correctional Facility for her role in a murder, in an August 2020 letter.
Research shows that long-term isolation—both among the general public and among inmates in solitary confinement—can cause anxiety, anger, depression, paranoia, psychosis and acting out. It can also exacerbate mental illness, which is one reason why Colorado has banned the practice of putting inmates with certain mental health conditions into long-term confinement.
This is also one reason why, in 2012, Tom Clements, a former director for the Department of Corrections, decided to close Centennial South, a prison built for solitary confinement in 2010. (With permission from lawmakers, Gov. Polis reopened the prison in 2020.) In 2013, Clements was shot and killed at his doorstep by a man who spent much of his eight years in prison in solitary confinement.
Clements’ successor, Rick Raemisch, described the assassination as one of the unforeseen consequences of solitary confinement. In a 2017 essay in The New York Times, Raemisch described solitary confinement as a form of “torture” that “manufactures and aggravates mental illness.” That same year, Raemisch enacted a policy seeking to cap solitary confinement at 15 days.
The policy was a significant step toward making prisons less traumatic. Williams, the Department of Corrections director since January 2019, sought to continue this trend when he made “normalization” his top priority. This means making prisons less about punishment and more about rehabilitation so that when people get out of prison, they are less likely to return.
Before the pandemic, people were painting murals, attending CrossFit classes, and getting work and job training through the state’s Take TWO program. The pandemic put an end to all this, said Jamie Amaral, a former prison guard at Sterling who worked on one of the state’s teams dedicated to brainstorming and implementing normalization as a policy.
During the pandemic, Amaral said, prison officials suspended family visits, eliminated outdoor time, and shut down job and education programs. She said these precautions are going to make it harder for people when they get out of prison.
“You’re going to dump them back into society after a horrible experience in which they were treated so poorly,” Amaral said in an interview. “They are being set up for failure.”
She added, “They talk about prison being rehab. You shouldn’t have PTSD and have to go to therapy to recover from it. People are going to have to recover from what they said was going to fix them.”
Determined to stay out of prison
Williams said normalization is still his top goal. He hopes to soon ramp up programs scaled back during the pandemic. He also wants to set up an email system so people can have more options to speak to their family, friends and loved ones. He said these programs will give inmates more “hope” and “purpose” to help deal with the effects of the COVID-19 lockdowns.
COVID-19 outbreaks continue to trigger movement restrictions in prisons. But the vaccine appears to be helping make outbreaks less common. As of May 17, about 74% of people incarcerated in Colorado’s prisons have received at least one dose of the COVID-19 vaccine, according to data from the Department of Corrections. In May, Williams said the vaccination rate among prison staff was lower, about 52%, despite a $500 incentive to take the vaccine.
Harter, who quarantined in Centennial South, is now incarcerated at the Arrowhead Correctional Center in Cañon City, a minimum-security prison where he expects to finish serving his sentence for attempted burglary. He said he’s vaccinated and working in the kitchen, something he said he dreamed about while he was isolated in Centennial South. He said he’s planning to see the parole board in June, and he thinks he has a good shot at getting out.
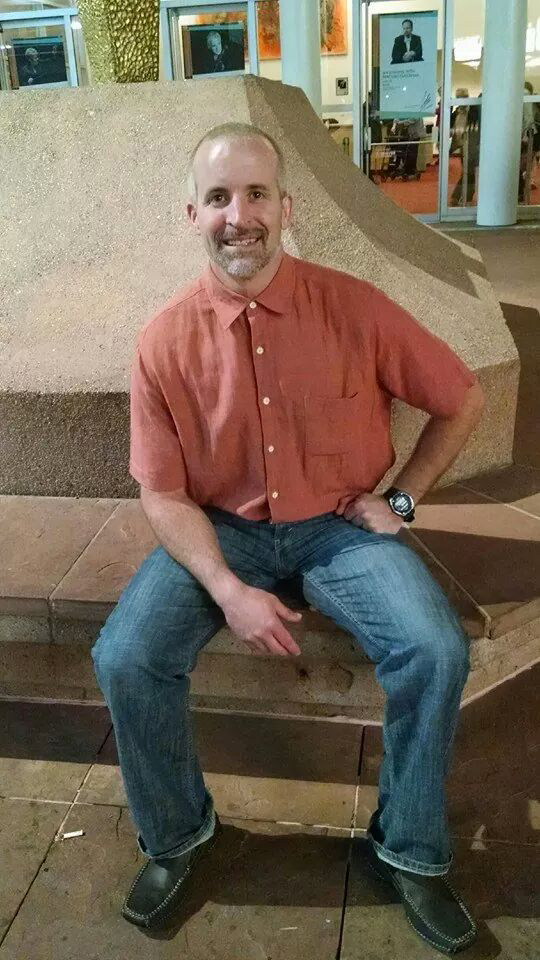
Matthew Harter in an undated photograph. Photo courtesy of Patricia Peel
When Harter does get out, he said he’ll have to monitor his sobriety. He’s been addicted to uppers, such as cocaine, and opioids, which he used to come down. He has trauma to work on, too. He said his son died of an overdose. And he recently had a bad breakup.
His time in prison is one more experience he has to deal with.
“I’m gonna try to use therapy and go to a support group. And just being able to live my life—going to work and being active—I’m sure will help,” Harter said. “I am determined to stay out of prison.”
Related story: For Incarcerated Youth, the Pandemic Isn’t Over Yet